[This post combines a summary of a recent survey into the global prevalence of diabetes, with a piece I wrote a few years ago on the topic, aimed at the AQA specification.]
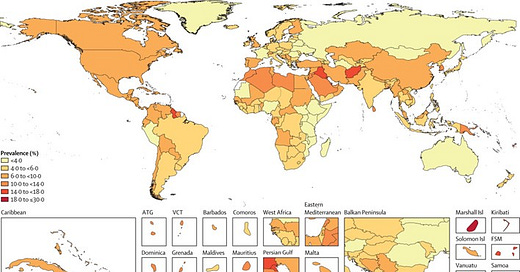
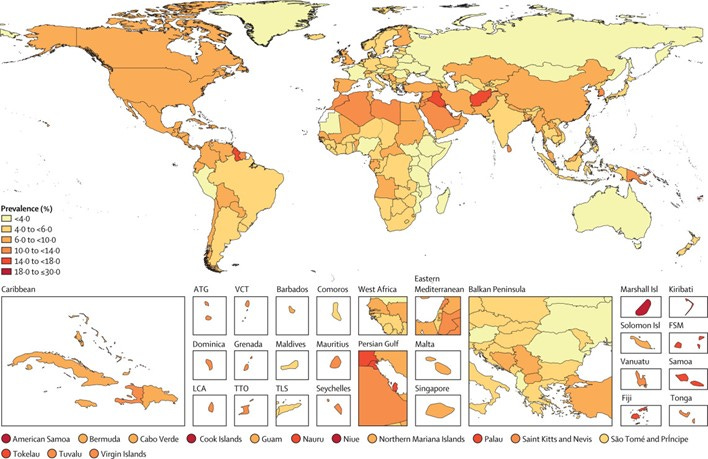
A recent study published in The Lancet found the number of people with diabetes has doubled over the past 30 years, totalling over 800 million worldwide, with the largest increases in low- and middle-income countries (Figure 1). This rise is linked to obesity, ageing populations, and economic hardship, with over half of diabetes cases concentrated in India, China, the USA, and Pakistan.
Despite accessible treatments, many low-income regions have low treatment rates, which are exacerbating health inequalities. Health experts urge ambitious policies to promote healthy diets, exercise, and improved healthcare access to prevent and manage diabetes effectively worldwide.
Figure 1 Age-standardised total diabetes prevalence rates in 2021
Type 2 diabetes is one of several non-communicable diseases (NCDs). There are two types of diabetes:
· Type 1 diabetes occurs when the pancreas does not produce insulin. It can occur at any age, but usually before the age of 40. It is usually treated with insulin injections.
· Type 2 diabetes (T2D) occurs when the body doesn’t produce enough insulin to function properly, or the body’s cells don’t react to insulin. It is much more common than Type 1 and is often linked with being overweight or obese.
Prevalence and distribution
According to the World Health Organisation (WHO):
· the total number of people in the world with T2D is projected to rise from 382 million in 2013 to 592 million in 2035.
· it is estimated that 80% of the people who have T2D live in developing countries
· T2D accounted for 11% of global health expenditure in 2013 ($548 billion), a figure expected to be over $600 billion in 2035
· T2D is associated with roughly 8% of total world mortality, about the same as HIV/AIDS and malaria combined
· Mortality and disability associated with T2D are particularly high in poor- and middle-income countries where people are unlikely to get the treatment that helps prevent the worst complications of the disease.
Links to the physical environment
Links between most, if not all, NCDs to the physical environment are difficult to establish. Scientists have tried to examine if there is a link with air quality in urban areas, and with varying temperature levels around the world. No such links have been established. Increased temperatures within an urban area, leading to heat stress, could add to the pressures already placed on a body due to being overweight or obese. Similarly, difficulty of breathing in a polluted environment could add further stress. However, these are both exacerbating factors rather than direct causes.
Links to the socio-economic environment
The WHO states that too much weight gain and obesity are ‘driving’ the global T2D epidemic. Recent estimates suggest that 1 billion people in the developing world are obese. There are several factors contributing to this:
· Diet: high calorie intake is the main factor leading to obesity. In developing countries rapid economic development has introduced a more ‘Western’ diet, with less fruit and fewer vegetables, combined with a higher intake of carbohydrates, fatty foods, salt and sugar.
· Urban lifestyles: rates of urbanisation in the developing world are considerably higher than elsewhere. Urbanisation tends to mean a more sedentary lifestyle, with a low level of physical activity.
· Tobacco use: smoking is a key risk factor linked to T2D: an estimated 50–60% of adult males in developing countries are regular smokers.
· Stress: stress increases blood sugar levels, raises blood pressure and can suppress the digestive process. Raised blood sugar levels are a key risk factor in the development of T2D.
Impact on health and well-being
Diabetes cannot be cured but can be managed with a mixture of medication and lifestyle change. Longer term it can lead to heart disease, kidney failure, blindness, and, in extreme cases, amputation of limbs. As most healthcare costs in developing countries must be paid by patients out of their own pockets, the cost of health care for T2D creates significant strain on household budgets, particularly for lower income families.
Management and mitigation strategies
Public awareness of T2D is slowly increasing in many developing countries. In Sri Lanka, for example, awareness is increasing mainly because of local media coverage and the activities of the Diabetes Association of Sri Lanka (DASL). DASL has a walk-in centre in the capital Colombo, where individuals can be screened or take part in structured health programmes at a modest cost. The centre also provides information through workshops, a website and printed materials. DASL is also spreading the message that exercise can help reduce the threat of T2D. Exercise areas are being created in many urban centres within the country.



Really interesting article. I was actually a little disappointed that AQA didn’t include any questions on health and the role of organisations in the exams this year given the global pandemic. I wish that the questions had more contemporary content at times. Maybe they do and I just don’t see it but I would like geographers to more fully engage in current affairs - cost of living crisis, fossil fuel dependency following Russias invasion of Ukraine etc.